Hemorrhoids (commonly known as piles) are a widespread anorectal condition that can cause pain, bleeding, itching, and discomfort during bowel movements. Advances in surgical technology have led to safer, faster, and less painful treatment options—one of the most significant being the Hemorrhoidal Stapler.
What Is a Hemorrhoidal Stapler?
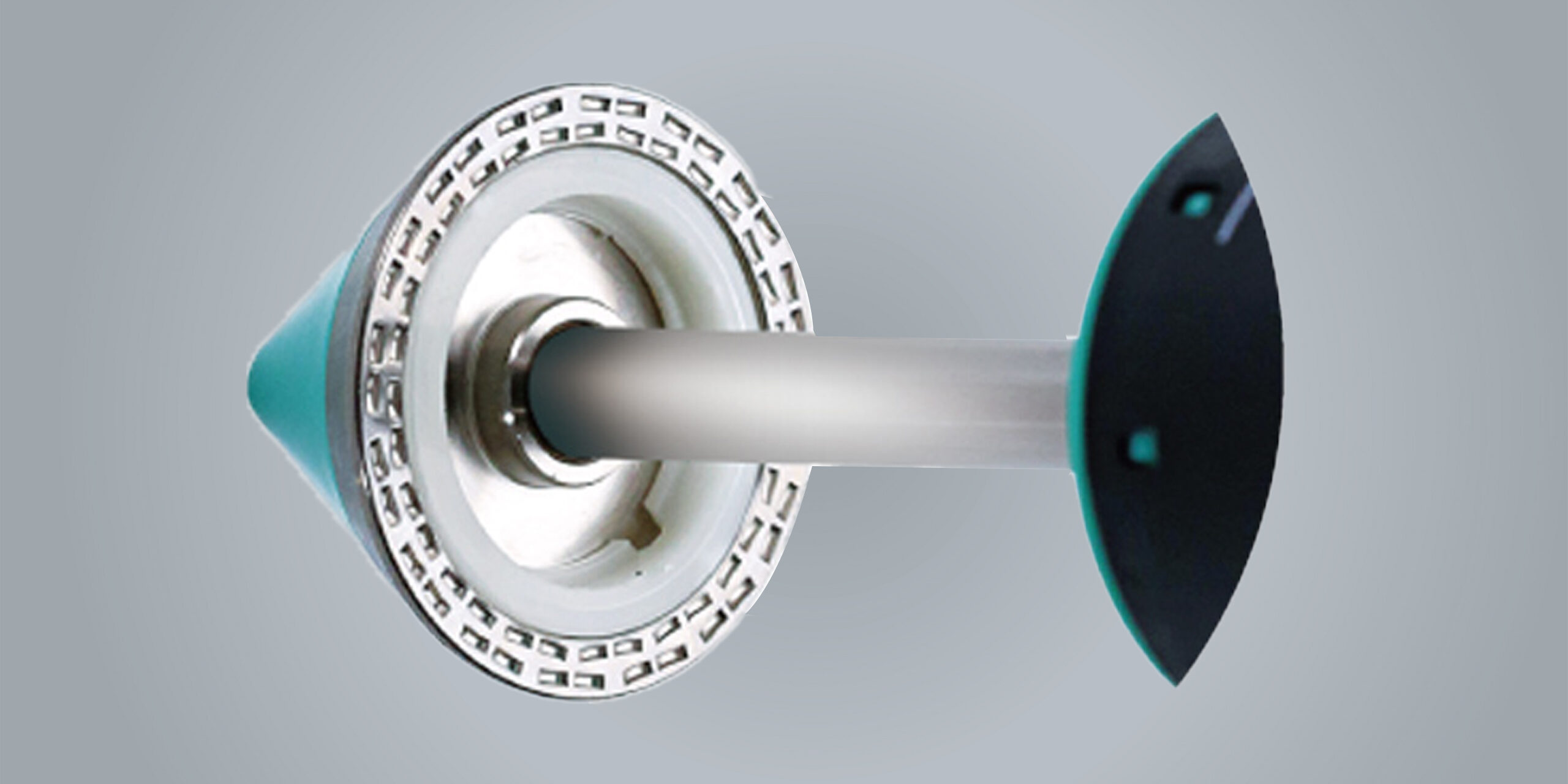
A hemorrhoidal stapler is a specialized surgical device used in a minimally invasive procedure called Stapled Hemorrhoidopexy (PPH – Procedure for Prolapse and Hemorrhoids). Unlike conventional hemorrhoid surgery, which involves excision of hemorrhoidal tissue, this technique repositions and reduces hemorrhoids by stapling the prolapsed tissue back to its normal anatomical position.
The device works by:
-
Removing a circular ring of excess rectal mucosa
-
Lifting prolapsed hemorrhoidal tissue upward
-
Cutting off excessive blood supply to hemorrhoids
-
Simultaneously stapling the tissue to promote healing
Why Is a Hemorrhoidal Stapler Used?
1. Minimally Invasive Treatment
The stapler operates above the dentate line, an area with fewer pain-sensitive nerves. This significantly reduces postoperative pain compared to traditional hemorrhoidectomy.
2. Less Postoperative Pain
Since no external hemorrhoidal tissue is cut, patients experience minimal pain, leading to improved comfort after surgery.
3. Faster Recovery
Most patients can return to normal daily activities within a few days, making it an ideal option for working professionals.
4. Reduced Bleeding
The stapling mechanism seals blood vessels during the procedure, minimizing intraoperative and postoperative bleeding.
5. Shorter Hospital Stay
Many stapled hemorrhoidopexy procedures are performed as day-care or short-stay surgeries, reducing hospitalization costs.
6. Lower Risk of Wound Complications
As there are no open wounds around the anus, the risks of infection, delayed healing, and wound-related complications are significantly reduced.
Conditions Treated Using a Hemorrhoidal Stapler
Hemorrhoidal staplers are most commonly used for:
-
Grade III hemorrhoids (prolapse requiring manual reduction)
-
Grade IV hemorrhoids (permanently prolapsed)
-
Prolapsing internal hemorrhoids
-
Rectal mucosal prolapse associated with hemorrhoids
⚠️ Note: Hemorrhoidal staplers are generally not recommended for external hemorrhoids.
Key Benefits for Surgeons and Patients
For Patients
-
Minimal postoperative pain
-
Faster return to work
-
Less need for pain medication
-
Improved quality of life
For Surgeons
-
Consistent and controlled tissue resection
-
Reduced operative time
-
Predictable clinical outcomes
Conclusión
A hemorrhoidal stapler represents a modern, patient-friendly approach to treating advanced internal hemorrhoids. By focusing on repositioning tissue rather than excision, this technique offers less pain, faster recovery, and excellent clinical outcomes. As minimally invasive colorectal procedures continue to evolve, hemorrhoidal staplers have become a preferred choice for both surgeons and patients seeking effective and comfortable hemorrhoid treatment.